Correct Layered Repair Of Third Degree Perineal Laceration
Perineal Lacerations As is the case with second degree laceration repairs, studies have shown that after episiotomy, using skin adhesive to close the perineal skin—after closure of vaginal layers, perineal muscles, and perineal body—results in no differences in reported pain and shorter procedure duration when compared with suturing (19 vs 23 minutes, p=.001). Because of the risk and infrequency of severe lacerations, these repairs should be completed by the most experienced physicians providing obstetric care. 20 the rectal mucosa is repaired using an.

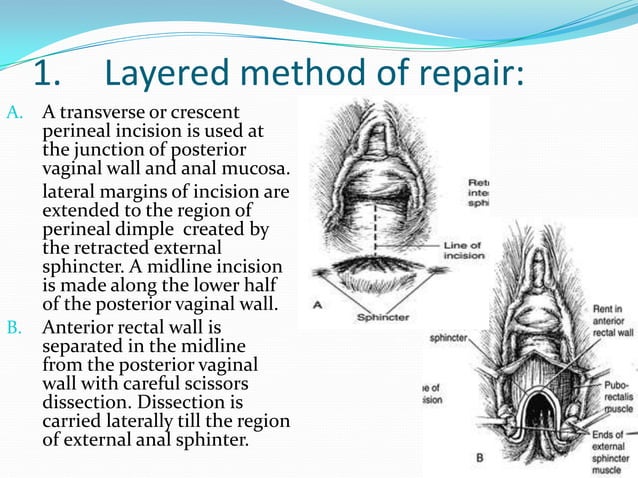
3rd Degree Perineal Repair Demonstration Youtube Experience some type of perineal laceration during vaginal delivery.1 third and fourth degree perineal lacerations can be a complication of vaginal delivery, especially in the presence of a midline episiotomy or an assisted vaginal delivery. correct assessment of the laceration and proper repair is necessary to reduce the. Repair of third degree tears. two methods exist to repair the external anal sphincter (eas): end to end technique . cut ends of the eas are isolated and brought to the midline end to end ; overlapping technique. cut ends of the eas are brought to the midline and lie atop one another ; only suitable for type 3c lacerations (the eas is completely. 3.3.4 step 2 suturing the perineal muscle layer 7 3.3.5 step 3 suturing the perineal skin 8 3.4 management following perineal trauma repair (1st & 2nd) 8 3.5 suturing of the third fourth degree tears 9 3.5.1 post third fourth degree tear procedure 11 3.6 suturing of rectal button hole tears 12 3.7 delivery management after previous 3rd 4th. Degree of laceration. description. first degree. superficial laceration of the vaginal mucosa or perineal body. second degree. laceration of the vaginal mucosa and or perineal skin and deeper subcutaneous tissues. third degree. 3a. second degree laceration with laceration of the capsule and <50% of the external anal sphincter muscle.

The Third Degree Perineal Laceration And Rectovestibular Fistulae In 3.3.4 step 2 suturing the perineal muscle layer 7 3.3.5 step 3 suturing the perineal skin 8 3.4 management following perineal trauma repair (1st & 2nd) 8 3.5 suturing of the third fourth degree tears 9 3.5.1 post third fourth degree tear procedure 11 3.6 suturing of rectal button hole tears 12 3.7 delivery management after previous 3rd 4th. Degree of laceration. description. first degree. superficial laceration of the vaginal mucosa or perineal body. second degree. laceration of the vaginal mucosa and or perineal skin and deeper subcutaneous tissues. third degree. 3a. second degree laceration with laceration of the capsule and <50% of the external anal sphincter muscle. Injury to the perineum during vaginal delivery can be classified into four degrees of laceration, 3 as described in table 62 1 and demonstrated in fig. 62 3.third and fourth degree perineal lacerations, also known as obstetric anal sphincter injuries (oasis), have been associated with dramatically increased rates of anal incontinence 5 to 10 years after delivery compared with a cesarean. Infections and wound breakdown may complicate laceration healing. risk factors for breakdown of a perineal laceration include operative deliveries, mediolateral episiotomy, and meconium stained amniotic fluid. 18 severe third and fourth degree lacerations are more prone to infection and break down. a single dose of broad spectrum antibiotics.
Comments are closed.